- 2008 E Hebron Pkwy Ste. 110 Carrollton, TX 75007
- +1 469-501-2224
PranapedicsTM, Comprehensive Sleep Medicine For Men & Women, Focused Woman’s Sleep, Sleep & Chronic Disease, Mission Critical – Aviation & Transportation Program, Military Airway Program and Martial Arts Airway & Spine Program


Sleep disordered breathing is a collective term which includes snoring, upper airway resistance syndrome and sleep apnea. Sleep apnea can be further divided into obstructive sleep apnea, central sleep apnea and mixed or complex sleep apnea.


Snoring can occur with air going through the nose, into the throat vibrates when in contact with structures or tissue in the nose or throat. Snoring can be mild to severe. There are multiple risk factors such as nasal congestion, deformed nasal tip, collapsed nasal valves, deviated septum, malocclusion, alcohol use, medication and obesity. A recent study showed that there is a high correlation between the severity of snoring and the severity of sleep apnea based on an AHI of on polysomnography.(Chiang, Lin et al. 2022)
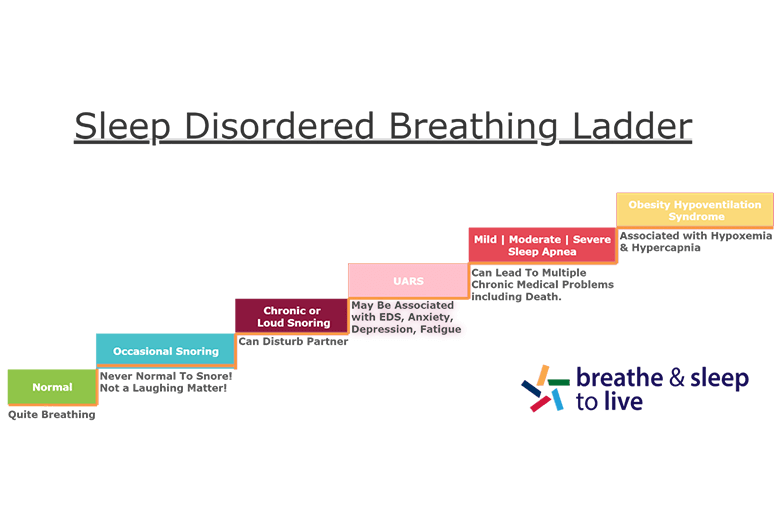
Upper Airway Resistance Syndrome is a condition that might be a precursor for sleep apnea. It may affect all ages. It has also been reported in young fit females. It is associated with insomnia and delayed sleep. Daytime symptoms can include fatigue and sleepiness.
Apnea-Hypopnea Index is less than 5 events/hr.
Once patient is diagnosed on a sleep study, then at trial of CPAP maybe tried along with a craniofacial workup to further ascertain the etiology of the problem and discuss other treatment options.
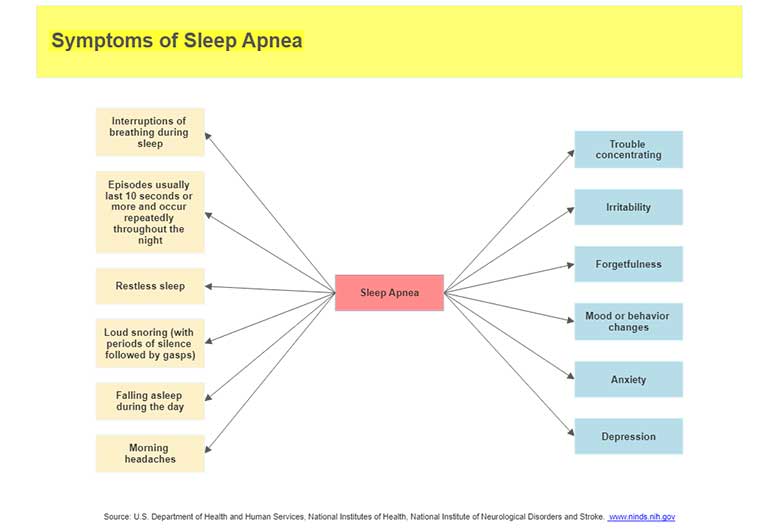
Sleep apnea is a common breathing sleep disorder where brief interruptions of breathing during sleep. The most common type of sleep apnea is obstructive sleep apnea (OSA). OSA occurs when the upper airway collapses or becomes blocked during sleep, thus reducing or stopping airflow into the epiglottis.

OSA is a serious condition that diminishes quality of life and is also associated with many common comorbid conditions.

It is estimated that the average life span of a patient with untreated OSA is 58 years, much shorter than the average life span of 78 years for men and 83 years for women.

You have difficulty either falling asleep or maintaining sleep through the night or you wake up unrefreshed even after sleeping 7 to 9 hours.
Insomnia – When To Seek Help from Primary Care Physician
You should discuss your sleep with your primary care physician or PCP on an annual basis. If you have any concern about your sleep at any time, please bring it up with your physician. Do not take sleep lightly. From a delusionary standpoint, humans would not be spending one third of their lifetime did not sleep if it was not necessary. Sleep may have a directive or restorative effect on the body. Therefore, it is imperative to sleep well. If not just for 8 hours but sleeping efficiently and without arousals, disturbances, sleep disordered breathing.
Insomnia Effects
Narcolepsy is a rare sleep disorder where a patient can fall asleep very easily. Narcolepsy Type I is associated with Cataplexy and Narcolepsy Type II is not associated with Cataplexy.


Hypersomnia is excessive sleepiness. Causes can be due to insufficient sleep, sleep apnea, medication or substance use, circadian rhythm or delayed sleep syndrome, shift work, periodic limb movement disorder, depression or other medical problems such as hypothyroidism, Parkinson’s disease or other neurologic disorders.
Primary sleep disorders that cause hypersomnia include Narcolepsy, Idiopathic Hypersomnia (IH), and Klein-Levin Syndrome.


RLS may present with symptoms of burning, aching, pain, cramping, tingling, creepy crawly feelings predominantly in the legs at night time.
RLS can be associated with End-Stage Renal Disease, iron deficiency and medications. Can occur with pregnancy.
Shift Work Sleep Disorder may occur in people who work differently daytime or night time shifts. This can be associated with difficulty falling asleep after a shift or feeling sleeping during the work shift. This usually happens as the shift may not coincide with the body natural circadian rhythm.

Chiang, J. K., et al. (2022). “Correlation between snoring sounds and obstructive sleep apnea in adults: a meta-regression analysis.” Sleep Sci 15(4): 463-470.